Benefits enrollment season feels overwhelming for most employees. They’re faced with complex plan comparisons, confusing terminology, and high-stakes decisions about their family’s healthcare, often with limited time and unclear guidance. While the complexity of benefits options will always exist, the enrollment process itself can be streamlined to reduce anxiety and help employees make informed choices.
The problem is that most organizations still rely on scattered systems and one-size-fits-all approaches that leave employees feeling lost and unsupported. When the process is confusing and hard to navigate, even the best benefits packages fail to deliver their intended value.
What is benefits enrollment?
Benefits enrollment is the annual process where employees select their healthcare, insurance, and other benefit options from their company’s offerings. It typically includes:
- Choosing medical, dental, and vision insurance plans
- Setting contribution levels for retirement accounts and flexible spending
- Updating beneficiary information and dependent coverage
- Making decisions about supplemental insurance and wellness programs
While this sounds straightforward, effective enrollment requires employees to understand complex plan differences, calculate costs, and make decisions that will impact their finances and healthcare for the entire year. When the process lacks clarity or guidance, employees often make suboptimal choices or skip enrollment altogether.
The challenges
For most organizations, the biggest hurdle is the fragmented nature of the enrollment experience. Open enrollment and life-event updates often happen in separate systems, benefits information is scattered across multiple documents, and employees struggle to access the process from different devices or locations.
Traditional enrollment approaches compound the problem. Generic communications fail to resonate with diverse employee needs, the process is difficult to pause and restart, and year-over-year changes aren’t clearly explained. Managers often lack the training and tools to support their teams, leaving employees to navigate complex decisions alone.
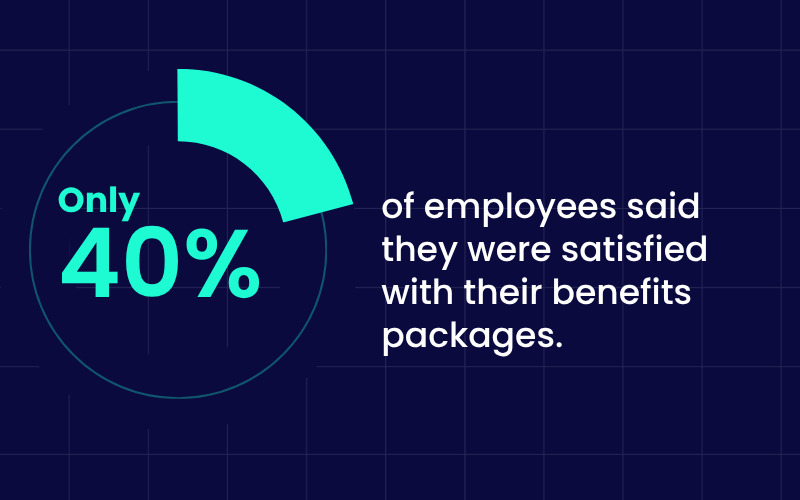
It’s no surprise that only 40% of employees said they were satisfied with their benefits packages in 2023. Without clear guidance and personalized support, even comprehensive benefits fail to meet employee expectations and organizational goals.
The Solution: WalkMe
This is where digital adoption platforms like WalkMe become game-changers.
Rather than forcing employees to hunt through PDFs and separate help resources, these platforms provide contextual guidance directly within the enrollment portal. WalkMe, specifically, offers step-by-step walkthroughs, plan comparison tools, and real-time support that helps employees understand their options and complete enrollment with confidence.
The results speak for themselves: organizations using guided enrollment workflows have improved self-service usage by 10% and reduced support time by 306 hours per year for every 1,000 employees. But implementation success depends on following proven best practices.
A practical guide for making benefits enrollment better
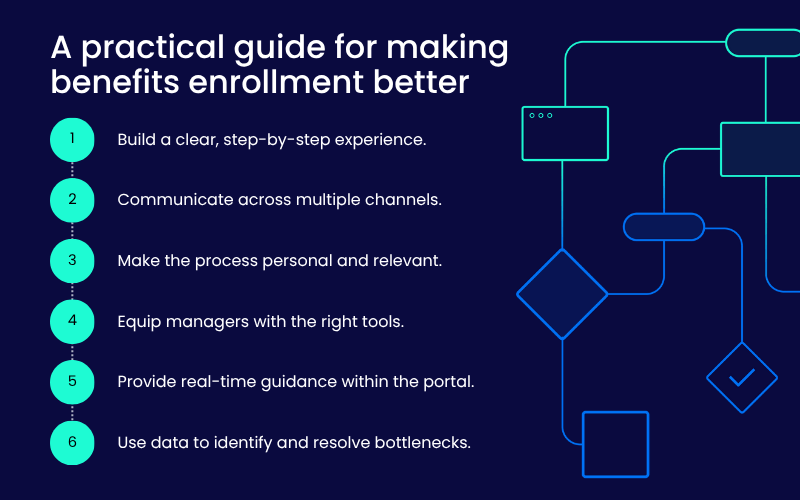
- Build a clear, step-by-step experience
Guided enrollment helps employees compare plans, understand options, and complete the process without second-guessing their decisions. Tools like WalkMe can provide interactive walkthroughs that allow employees to pause and resume, highlight year-over-year changes, and offer explanations exactly when needed.
- Communicate across multiple channels
Multi-channel communication keeps employees engaged throughout the enrollment period. Email reminders, mobile alerts, intranet messages, and in-app prompts work together to ensure important deadlines and updates don’t get missed, regardless of how employees prefer to receive information.
- Make the process personal and relevant
Personalized enrollment experiences show employees only what applies to their situation. This might mean highlighting dependent coverage options, providing cost calculators for different scenarios, or suggesting plans based on previous selections and life changes.
- Equip managers with the right tools
Managers play a crucial role in supporting their teams through enrollment, but they need proper resources. Digital guidance can provide managers with dashboards to track team progress, talking points for common questions, and alerts when team members need follow-up.
- Provide real-time guidance within the portal
In-app support eliminates the need to switch between enrollment systems and help resources. WalkMe can deliver tooltips, explanations, and decision-support tools directly within the benefits portal, reducing confusion and helping employees make informed choices in the moment.
- Use data to identify and resolve bottlenecks
Analytics from guided enrollment platforms help HR teams see exactly where employees get stuck, which plans cause confusion, and when additional support is needed. This data enables continuous improvement of the enrollment experience.
Putting it all together
The combination of these strategies creates a comprehensive enrollment ecosystem. When implemented effectively with platforms like WalkMe, HR teams can track completion rates, identify common pain points, and continuously refine the experience based on real employee behavior.
Although by 2025, 70% of employers offered multiple medical plans, making clear comparisons more important than ever, many organizations still rely on outdated enrollment approaches. WalkMe bridges this gap by ensuring employees can navigate complex choices with confidence and complete enrollment successfully.
What success looks like
When benefits enrollment is done well, the benefits are clear:
- Higher self-service usage and fewer support tickets during enrollment periods
- Increased enrollment completion rates and reduced coverage gaps
- Better employee satisfaction with both the process and their benefit selections
- Significant time savings for HR and support teams
Organizations that invest in improving enrollment create lasting impact beyond the annual enrollment period. With mobile-responsive self-service usage rising from 43% to 69% in similar programs, and organizations reporting 40% drops in support requests and 45% higher satisfaction scores, streamlined enrollment becomes a competitive advantage that demonstrates genuine care for employee experience.

